Consortium Physiotherapy Hull's : Guide to Acute Lower Back Pain and Sciatica
A C U T E L O W E R B A C K P A I N A N D S C I A T I C A G U I D E
Public beliefs on back pain are often incorrect (source) while our approach to managing back pain in the past also hasn’t worked very well. Fortunately, we now have a much more contemporary understanding of how to best manage things (source).
If you are suffering with recent onset lower back and/or sciatica then this article should help you guide your care. If you have developed back pain for the first time then research has shown that simple advice can reduce your pain and help prevent re occurrence (source). THIS IS NOT A GUIDE FOR THOSE WITH CHRONIC LOWER BACK PAIN.
Terminology
What do we mean by lower back pain: Pain, soreness or stiffness anywhere between the rib cage to the top of the buttocks.
Acute back pain: Symptoms that are new and started usually within the last 6 weeks.
What is sciatica: This is pain radiating down one or both of your legs usually as a result of the nerves in your back being irritated, this can often be associated with numbness and tingling and in some instances weakness.
Should be worried that something serious is causing my symptoms?
It is difficult to identify a clear single cause of lower back pain. In most cases it is usually a combination of things that has led to you becoming symptomatic. There are in some very rare cases specific and serious causes of your back pain such as infections, fractures, tumours and sometimes inflammatory diseases but the good thing is that these things are usually only present in less than 1 out of every 10 people.
Interestingly back pain is not often caused by prolonged sitting (source), repetitive lifting or bending (source).
There is little evidence that disc bulges or degenerative changes are the cause of back pain (source). Some disc bulges can cause back pain and leg pain but fortunately the majority of these heal up and are resorbed naturally (source).
What does the future hold for me if I have acute back pain and/or sciatica?
Back pain with or without sciatica is very common and makes up a large proportion of what we see in the consortium physiotherapy clinic. In some cases this can be triggered by certain activities or by specific movements but in other cases there is no obvious reason. Back pain is quite common amongst the general population and most people will suffer multiple episodes of back pain at some point in their lives. The good thing here is that in most people this usually improves given time and then you can get back to normal without any long term issues. Having sciatica is often a sign that the nerve is also irritated but again the majority of this gets better on its own given time.
What should I do then?
There is lots of research and guidelines that have been developed nationally in recent years to help tell us the best way to manage your acute symptoms. In the first instance self care is always the most effective and cheapest option available. We would advise that you carry on as best as possible within the limits of your pain and continue to participate in your normal activities and carry on at work if possible. This usually helps quicken your recovery and helps avoid persistent symptoms. At first you may be struggling to move about freely but as the days pass this usually gets better. You should then build things back up in a sensible and GRADUAL manor. Only if you are in very severe pain and have no choice would we recommend resting in bed as this often results in your symptoms taking longer to get better. It s often best to treat your back exactly the same as you would if you had sprained your ankle. For example, you wouldn’t stress to much about it to begin within, you would use it as your pain allowed and then gradually get back to normal over the coming weeks as it heals up. Often if we use the same to our back and leg pain it can be helpful.
It is always useful to remember that the amount of pain you experience in your back and/or leg rarely equates to the level of damage or harm that you have done. Similar examples of this can be seen when you have a tiny paper cut with a large amount of pain.
Most people don’t need a large amount of treatment in the early stages and you are often discharged following a single session. If you do not improve or should you worsen further we would strongly recommend you come back for further sessions to help us optimise your care. If we do see you in the clinic we will try to screen out people with higher levels of pain, distress, anxiety and fear of movement as we would provide these individuals with more face to face input at early stage to give them a better chance of recovery.
What exercises should I do?
We are strong believers that exercise should be focused around what you enjoy most. Your spine is full of joints and is a highly flexible structure and therefore likes to move freely in all directions. Exercise tends to work best when performed over long periods of time. For this reason you are encouraged to choose the type of exercise that you enjoy most and the type that fits in best with your lifestyle. It is best to exercise in the long term with the reassurance and understanding that stiffness and soreness after exercise is often normal and over time this becomes less. To begin with you may have to move in a guarded and cautious way as your pain will still be prominent at this time. As you start to improve we would recommend trying to move more freely again. We often encounter patients who have spent years deliberately bracing and protecting their spine and moving rigidly. In the majority of cases this is not always a helpful strategy, instead it can often lead to higher levels of pain, stiffness and disability.
medication advice
Guidance from NICE in 2016 (source) recommends using Non Sterioidal Antiinflamatory Drugs (NSAIDs) for managing back pain at the lowest effective dose and for the shortest possible period of time. If you can’t take NSAIDs then weak opioids can be used on the same basis. We would recommend you must take advice from your physio, GP or pharmacist if you are considering medicating.
The guidelines recommend against using paracetamol alone for managing back pain and to not advise that you are routinely offered opioids.
If you have severe sciatica then a number of neuropathic medications can be considered including amitriptyline, duloxetine, gabapentin or pregablin. Again you will need to discuss this with a medical practitioner and you should not take these medications if you have back pain alone.
Lots of physiotherapy practices offer all sorts of treatments like acupuncture and manipulation. Should I pay for these things?
The guidelines of excellence recommend AGAINST treatments including belts, corsets, acupuncture, stand alone manual therapy, foot orthotics, traction and electrotherapy including ultrasound, TENS, PENS and interferential. This is because their effectiveness is limited and therefore in general they are not considered to be cost effective across the board. Treatments like this can also leave patients with negative back pain beliefs and an increased reliance upon therapists to ‘fix’ their back pain, leading to worse outcomes in the long term.
Can my spine or pelvis end up out of alignment or out of place?
Despite the fact that many patients are still treated for this, there is no evidence to back up the idea that you can end up with your spinal joints or discs being out of alignment. Usually if you have your back manipulated it can provide short term pain relief but this is because it manipulates your nervous system rather than someone putting something back in place. Some patients do naturally have different spinal postures but this may only mildly pre dispose you to some lower back pain and cannot be treated by manipulation or ‘realignment.’
Who is at risk of developing longer term back pain and what can be done?
Individuals who become extremely fearful of moving, take excessive rest, avoid normal activities, cannot control their pain or who believe that something is seriously damaged in their back often are more likely to develop long term back pain. Given that the public’s understanding of back pain over the years has been incorrectly focused around the vulnerability of the spine we can easily see why some people end up in this difficult situation. A simple examination can help identify this group of patients and fortunately there are some strategies we can try to use to improve their situation. The best approach that we know is to identify various physical, cognitive, emotional and lifestyle factors that we feel could contribute to their ongoing pain. We will also look to identify and stop unhelpful pain behaviors and re introduce exercise alongside positive back pain beliefs and cognitive behavioral therapy. The success rates for this type of treatment can be very good but there are also a small group of patients that will fail treatment and require referral on to a higher level pain management and rehabilitation program.
When should I seek medical help?
If your back or leg pain gets worse not better and/or persists for longer than 6 weeks you should seek help. A simple assessment and face to face discussion should be enough to optimise your care in most cases. In this scenario we may discuss together how is best to proceed and in some instances we will arrange imaging if appropriate and refer you onto a spinal surgeon. The primary aim of surgery is usually to relieve sciatica and often leaves your lower back pain unaffected if not worse.
However, there are circumstances where you should seek help sooner, for example if you are known to be osteoporotic or if you experience unsteadiness or difficulty co coordinating/ controlling your legs when you walk. If you have intractable sciatic pain and cannot cope then it would also be sensible to seek help.
Should I ever seek EMERGENCY help?
It is rare to have to seek emergency care for lower back pain and/or leg pain. However if you experience any of the following symptoms should present to your local emergency department as a matter of urgency (source).
· Saddle anaesthesia (loss of feeling between the legs, numbness in or around your back passage or genitals).
· Bladder disturbance (inability to urinate or difficulty initiating urination, loss of sensation when passing urine, inability to stop of control urination, loss of feeling your bladder is full).
· Bowel disturbance (inability to stop a bowel movement, constipation, numbness when passing a bowel movement).
· Sexual problems (inability to achieve an erection or ejaculate, loss of sensation during intercourse).
· Severe sciatica associated with worsening neurological weakness for example an inability to lift your foot up from the floor.
Imaging
Imaging is often not helpful in most cases of lower back pain. Most of the degenerative changes found on MRI are often meaningless or incidental as these changes are usually similar to people of the same age that have no back pain. Often the ‘wear and tear’ that is seen simply reflects the normal aging process and shouldn’t be much cause for concern.
There are a small number of people who have symptoms that may require us to order you an MRI scan and this decision can be made after one of the Consortium Physiotherapists has performed a simple assessment. Imaging is helpful if
· you have any of the emergency symptoms listed above
· if you have persistent sciatica for longer than 6 weeks without improvement
· if in some rare cases you have severe, unrelenting and intolerable sciatic pain
will i ever need to have surgery?
Surgery in your lower back is reserved for patients with either severe nerve pain into their legs and/or patients who have developed neurological compromise (as is detailed in the section above titled when should I ever seek emergency help). Persistent sciatica that fails to improve over time is usually investigated with an MRI scan and dependant on the scan findings you may be referred for a surgical opinion. In rare cases of acute severe and uncontrollable sciatica you may be investigated urgently. Even then surgery is used primarily to relieve pressure on nerves and would be likely to leave your back pain unaffected if not worse. The guidelines state there is virtually no role for surgery for back pain whether it is acute or chronic. This is because the outcomes are usually poor. In some spinal centres they will operate for back pain but only if you are part of a special trial.
There is a lot of evidence that patients with more positive beliefs and a greater understanding of their symptoms have a better prognosis (source). We therefore hope that you have found this guide to be a useful resource.
If you would like to download this guide as a printable PDF then please click here.
If you need any more information then please do let us know by contacting us using contact@consortiumphysio.co.uk
The Ten Benefits of Massage Therapy & Sports Massage
Does stretching actually prevent injury?
Our worst nightmare as a runner or athlete is getting injured. We often try all kinds of methods to prevent this…
What do we think actually causes injury?
Do the traditional things we do to prevent injuries like stretching actually help?
A study carried out by Saragiotto et al, 2014 (SOURCE) found runners to believe that not stretching both before and after their run would leave them more likely to get injured. This is something that is commonly discussed in the Consortium clinic with our clients. We therefore felt this to be an important topic for us to provide an evidence based opinion on to help our clients separate fact from fiction.
Can static stretching reduce my chances of getting injured?
Static stretching (holding a position to stretch a muscle for a sustained period of time) historically has been a routine of many runners/athletes prior to beginning their activities to prevent against injury. However.... more recent evidence has suggested it’s maybe not as worth your while as you first thought! Lauersen (2013) (SOURCE) found static stretching did not have any protective effects with no support found for stretching and preventing injury when carried out either before or after activity. In fact.... it has also been suggested it can instead have a negative impact on the level of your performance! Did you know static stretches held for 45 seconds or longer, prior to activity can reduce maximal strength, power and muscular explosive performance, such as when jumping and sprinting? (Simic, 2012) (SOURCE).
OK...... So 45 seconds is a long time to hold a static stretch…
So what if I stretch for a shorter time?
Static stretching for shorter periods has been less associated with the previously mentioned negative effects but still has no benefit towards injury prevention, this may lead you to ask whether it is worth your time doing both before and after exercise?
Should I continue to stretch? Or is there a better alternative?
One thing we do know is that gradual muscle strengthening has demonstrated the ability to reduce sporting injuries by 1/3 and over-use injuries by a 1/2 (Lauersen, 2013) (SOURCE). More recently, specific eccentric muscle strengthening (working the muscle as it lengthens) has also been shown to both improve and gain long standing muscle length through a process of ‘sarcomeregenesis’ (increasing amount of contractile units in the muscle) (O’Sullivan, 2012) (SOURCE).
So what does this actually mean? In essence, if we included and carried out a specific graded eccentric muscle strengthening routine as part of our weekly training schedule we can ‘kill two birds with one stone’. By not only improving strength, which is proven to reduce the likelihood of injuries, but also by improving your flexibility at the same time if this is one of your aims. An example of this has been demonstrated with studies around the hamstring muscles suggesting an increase in muscle fascicle length by 1/2cm by using eccentric strengthening can reduce the chances of injury by up to 70% (Askling, 2014) (SOURCE).
But I feel better after stretching… so Should I stop doing this or carry on?
Often clients have carried out static stretches as part of their routines and ’rituals’ before races/competition/games for many years and it makes them feel good and ‘ready to go’… So if you feel happier continuing to do this it is perfectly O.K, although as we have discussed there is no evidence towards preventing injury and holding them less than 45 seconds should have no negative effects on your performance.
An alternative that you also may be aware of is dynamic stretching (using controlled movement and momentum of the body part e.g. whilst standing raising your knee towards your stomach then back to it's starting position repeatedly in a controlled manner to move the muscle from one end of its range to the other). Although this again has little evidence towards injury prevention. Instead, it may be more suited and is recommended to be included in a warm up to gradually prepare your body for the activity in hand (Behm, 2011) (SOURCE).
However, it is also worth mentioning that if your sport requires your joints to achieve sustained extremes of movement such as in Ballet or Kick boxing then static stretching is recommended to be carried out before in short duration to prevent impairment (Behm, 2011) (SOURCE).
Summary…
To summarise, static stretching before activity is something we have done for many years with the feeling it would ‘stop us pulling a muscle’, but surprisingly the evidence towards this is in fact pretty poor. A better alternative to prevent injury is suggested to be a gradual eccentric strengthening routine included in your weekly training plan. But as mentioned above this is not to say you can’t ever carry out static stretches again… As even though this is maybe not doing what we thought it was to prevent injury, it is not going to do you much harm either.
Hope you’ve enjoyed reading our latest ‘blog’… If you have any questions or would like any further information such as, how to implement a specific eccentric strengthening routine please don’t hesitate to contact us via our Facebook page, Website or telephone and one of our team will be more than happy to help. Also if there are any specific topics you’d be keen for us to cover in our next installments of our blog please let us know.
Kind regards,
The Consortium Team
Are you in need of a modern approach to manage your persistent lower back pain?
Looking for a modern and revolutionary approach to treating lower back pain? Tried every treatment before with no improvement..?
Most people with severe non specific chronic lower back pain (back pain with no specific structural cause found) have two things in common, they usually have severe pain and also a lack of function. Many of them have undergone treatments including manual therapy, exercise therapy, core exercises, stabilising exercises, manipulation, electrotherapy, massage, pilates, yoga , medications, injections etc (the list goes on....). The evidence base for management of back pain has evolved immensely over the last decade but despite this many patients continue to be treated with all of these traditional therapies with little effect.
Even the latest national guidance from NICE (National Institute for Health and Care Excellence) clearly state that practitioners should not be offering acupuncture, injections and electrotherapy for treatment of lower back pain (source).
Frustratingly, these types treatments are still marketed and sold to people in pain on a daily basis. There is therefore a clear need for physiotherapists, doctors, surgeons, osteopaths and chiropractors to improve the quality of what we offer for conservative management of non specific lower back pain and in the process move to a more contemporary approach.
(USEFUL ARTICLE TO READ ON NEED FOR DRASTIC CHANGES IN CURRENT MANAGEMENT OF LOWER BACK PAIN)
Since its inception, the Consortium clinic has always listed Cognitive Functional Therapy as a service provided for its patients. The research has shown this approach to be significantly more effective than any previous approaches we have traditionally used to manage back pain (source). This is exciting news for the future for those of you who suffer from severe disabling back pain.
What is Cognitive Functional Therapy (CFT)?
When it comes to treating lower back pain - a one size fits all approach simply does not work.
CFT is most importantly patient centred. This means it is focused entirely around you as a person, your life and your goals. CFT looks at the way you move and analyses some of the strategies you have adopted as a result of living in pain. It targets the fears and beliefs that are associated with performing spinal movements and the movement behaviours you often display around your back. It will help you understand that pain will not necessarily cause your back any damage. We will look through your MRI scan with you and help you to dethreaten some of the worrying things you may have been told about it. CFT will try to get you out of the vicious circle that so many patients find themselves trapped within. Often all of these things lead to a significant increase in the tension around your back and this often drives the nervous system to be over sensitised.
CFT will look to undo and change many of these things to provide you with better strategies to ease your pain and lessen your disabilities. It will help empower you to get back to doing the things in life that are of value to you.
What does the research say that Cognitive functional therapy achieves?
The trials for CFT suggest that this approach is far more effective than the traditional management of being manipulated, mobilised or exercised. It has been shown to significantly reduce peoples levels of pain, disability and fear of movement. It often improves your mood and mental wellbeing. Patients who have had CFT often have less need for ongoing treatments or time off work (source).
Is Cognitive Functional Therapy appropriate for everybody?
CFT can be applied to the majority of back pain. It is most appropriate for people with non specific back pain that is provoked by certain movements, postures or activities (85% of back pain). It is often even more appropriate for the more complex and disabled patients. It is also used successfully for those people with mild to moderate levels of back pain. However, CFT is not for everybody..... there are some patients (less than 15%) who have had a very specific structural cause of lower back pain identified, this approach is still beneficial but may focus on specific structural cause of symptoms aswell as all of the other contributing factors.
Want to learn more?
This video interviews one of the key researchers in CFT, it discusses what cognitive functional therapy actually is and the significant effects it can have....
Interested?
The Consortium clinic believes strongly in the use of the CFT approach for lower back pain. Should you wish to discuss with one of our clinicians then please contact our enquiries line on 01482 847705. We can always schedule one of our spinal specialists to ring you if needed. Alternatively you can email us at enquiries@consortiumphysio.co.uk
PART TWO - Managing load to avoid injury: How to not wrap yourself up in cotton wool
Welcome to the latest edition of the CONSORTIUM CHARTERED PHYSIOTHERAPISTS blog. Thank you for reading part 1 of ‘managing load to avoid injury’... If you have not read it yet and want to reduce your risk of injury then please click here to do so!
This article has been written by myself (Chris John) and another fellow Physiotherapist and friend Rob Parkinson. Rob is highly skilled physio and works in elite rugby alongside running his own private practice in Gloucester called Pro Performance. You can follow us both on twitter @chrisjohnphysio and @properformrehab
After reading the first blog you will have summarised a few points:
- The optimal amount of load is best for getting fit and trying to avoid risk of injury. Overloading or under loading can result in an increased risk of injury (Dye, 2005).
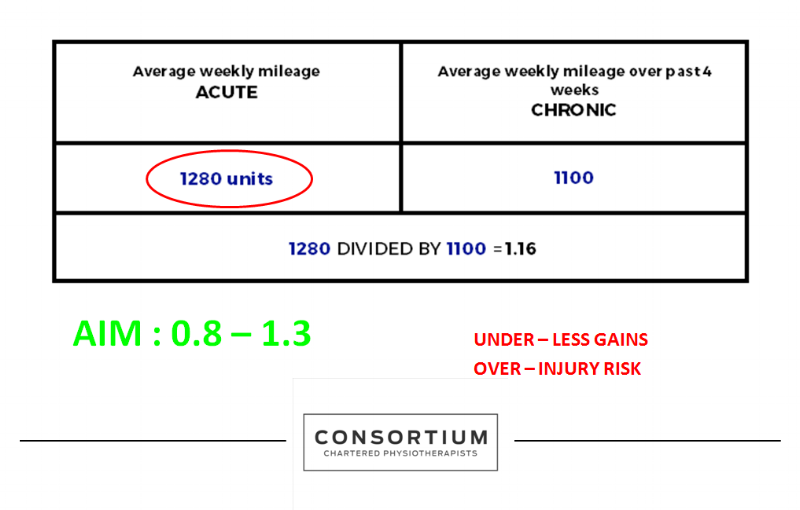
- The acute to chronic workload load ratio is a useful method to monitor your training and ensure you are not over or under loading. The ideal ratio is 0.8 to 1.3 (Gabbett et al, 2016).
Calculating your acute:chronic ratio will help prepare you for competition, improve your performance and should decrease your risk of injury.
My previous blog explains how to use this in a very simple way and is relatively easy to remember. However, the disadvantages to using a simple version like this is that everybody is different. Some of us are tolerant enough to be able to drastically increase our training and not end up getting injured. Some will find the opposite and only need to make small changes and often end up with problems. Some amount of this you cannot control, it will just depend on how you were put together and is simply the way you are. However... there are other factors that will influence how quickly you can progress. Things like your past medical history, age, weight and previous training levels will all have some influence. Using the simple acute to chronic workload ratio that we previously described in part one unfortunately does not account for any of these factors. The other downsides of keeping to a very simplistic model is that it is also very objective as it focuses purely on distance or volume of training and doesn't take into account how hard you went.
For this reason I present to you a more advanced way of calculating your training progression and I will go on to explain this below.
THE ADVANCED VERSION
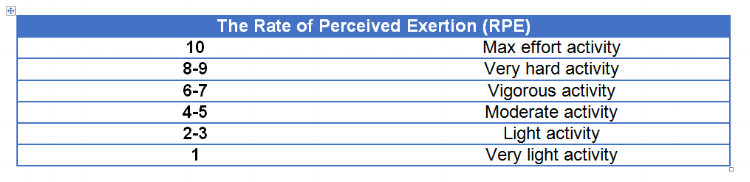
Uses Rate of Perceived Exertion (RPE) (ie 0 no effort, 10 maximum effort)
Calculate your time spent training into units ie. (RPE x number of minutes you undertook that activity for)
You then CALCULATE THE TOTAL FOR THE ENTIRE WEEK
So what is a rating scale?
The ‘Rate of Perceived Exertion’ is a well-known tool in the world of professional sport that is used to measure how the athlete perceives the intensity of workload given (Brito et al, 2016).
THIS CAN BE a game, running, cycling, training, strength and conditioning session, gym session and so on…
The Table below shows the Rate of Perceived Exertion scale.
So how do you work out your acute:chronic ratio using RPE?
You multiple your RPE by the training session time in minutes
(RPE x training session time = units)
EXAMPLE: A 30 minute gym session was an intensity of 7/10 (30 x 7 = 210 units)
You then use this to work out your total units for the acute and chronic weeks
ACUTE LOAD DEFINITION: The sum of load over 7 days
CHRONIC LOAD DEFINITION: The average acute load over the previous 4 weeks (or however many week you chose)
The following example demonstrates how you would calculate the total volume of units for one week of training
you then use this to work out your figure to see if you are in the safe zone or whether you are at risk as demonstrated below
SO LETS RECAP THE BENEFITS OF USING THE ADVANCED VERSION
- It takes into account internal and external factors as YOU score how YOU feel after that specific session (Coutts et al, 2004).
- How YOU progress is then specific to you only (Abbiss et al, 2015). For example, using a prescribed marathon website training program will provide you only with a generic protocol. It is not designed exactly for YOU and does not take into account any of the factors that will affect how quickly you can progress in comparison to someone else.
- You are in then in total control of your own programme; progressing yourself in a SMARTER way, trying to ensure you always work in your ‘sweet spot.' This will leave you better prepared for competition and less likely to get injured (Gabbett, 2016).
So remember, train hard…but train smart!
Thank you for reading.